Indian skin is particularly susceptible to hyperpigmentation. Most people in India have a skin tone ranging from Type III to Type VI on the Fitzpatrick scale, although Type II is also seen in the northernmost regions of the country. The general recommendations on reducing hyperpigmentation in people with darker skin are not alway set in stone when it comes to South Asian skin.
Something that will work in African American skin might not work as well in Indian skin. On a side note, South Asians tend to have substantially more body hair than other ethnicities, so laser hair removal is extremely popular in the subcontinent. Lasers that work well on the fairer skinned Indians (skin Type III or even lighter).
Treating Hyperpigmentation in Indian Skin
If you have Indian skin, you must check out the clinics and doctors that are listed in the India country section in my page on top clinics for dark skin laser treatments. Not only are these clinics experienced at treating darker skin, they almost entirely specialize in treating Indian patients.
Most of them have years of experience in using lasers to treat Indian skin. Whether for hair removal, hyperpigmentation treatment, acne scar revision, moles and skin tag removal and much more. And they all use the latest available technologies that work on South Asian dusky skin tones.
The depth of hyperpigmentation is also an important factor when it comes to treatment strategy. Epidermal hyperpigmentation is on the upper layers of the skin and hence easier to treat. In contrast, dermal pigmentation runs much deeper and requires more intensive treatments.
Vogue India has a good summary of recommendations in treating dark spots in Indian skin. According to Dr. Lara Devgan, if done too agressively, lasers, chemical peels, and microinfusion microneedling for fading darkness can make dark spots worse in peple with olive and darker skin tones.
The Ageless Clinic in India in Mumbai has a useful page that discusses pigmentation issues in Indian skin. Below is an image from the clinic’s instagram that shows a before and after result in removing hyperpigmentation from an Indian person.
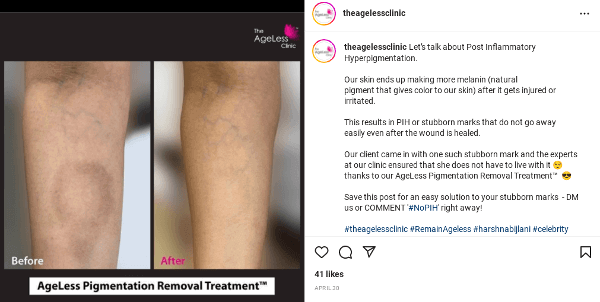
The clinic’s owner is Dr. Harsha Bijlani. According to her, once the issue causing your pigmentation is under control (whether hormonal, due to injury or excessive sun exposure), peels and lasers are the most common ways to prevent and fight pigmentation. Inititial treatment will usually consist of skin lightening creams that are more suitable for darker skin.
At the Ageless Clinic, hyperpigmentation treatment consists of the following options:
- PicoSure®.
- Clear Skin Laser™.
- Cosmelan™.
- AgeLess Diamond Skin Resurfacing™.
- Dermaroller with Lightening Agents.
- Mesotherpy with Lightening Agents.
- Skin-brightening Super-Medi Facials.
- AgeLess Stem Cell Face Treatment™.
- Chemical Peels.
A Common Skin Concern
Hyperpigmentation is a common skin concern for individuals with Indian skin tones. It can be caused by various factors, including sun exposure, inflammation, hormonal changes, and genetics. Here are some general recommendations for treating hyperpigmentation on Indian skin:
- Sun Protection:
- Sun exposure can exacerbate hyperpigmentation. Use a broad-spectrum sunscreen with a high SPF (at least 30) every day, even on cloudy days. Reapply sunscreen every two hours, especially if you are outdoors.
- Topical Skin Lightening Agents:
- Ingredients such as hydroquinone, kojic acid, niacinamide, alpha arbutin, and licorice extract can help lighten hyperpigmented areas. These ingredients may be found in over-the-counter products or prescribed by a dermatologist.
- Retinoids:
- Retinoids, such as retinol or prescription-strength tretinoin, can promote skin cell turnover and help fade hyperpigmentation. Start with a lower concentration to minimize irritation, and gradually increase if tolerated.
- Vitamin C:
- Vitamin C is an antioxidant that can help brighten the skin and reduce hyperpigmentation. Look for serums containing stabilized vitamin C (ascorbic acid) for maximum effectiveness.
- Chemical Peels:
- Chemical peels, including glycolic acid or salicylic acid peels, can help exfoliate the skin and reduce hyperpigmentation. However, these should be done under the supervision of a dermatologist to avoid complications.
- Microneedling:
- Microneedling involves the use of tiny needles to stimulate collagen production and improve skin texture. It can be effective in treating hyperpigmentation when performed by a trained professional.
- Prescription Medications:
- Dermatologists may prescribe stronger medications, such as topical steroids or combination creams, depending on the severity of hyperpigmentation.
- Avoid Irritants:
- Avoid harsh skincare products and treatments that can irritate the skin, as inflammation can worsen hyperpigmentation in individuals with Indian skin tones.
- Hydration:
- Keep your skin well-hydrated. Moisturizing regularly helps maintain the skin barrier and can contribute to an overall healthier complexion.
- Consult a Dermatologist:
- If hyperpigmentation is persistent or severe, it’s essential to consult a dermatologist. They can assess your skin, determine the underlying causes, and recommend a personalized treatment plan.
Remember that consistency is key when treating hyperpigmentation, and results may take time. Additionally, protecting your skin from further sun damage is crucial to preventing the recurrence of hyperpigmented areas. Always patch test new products and introduce them gradually to avoid potential irritation. Individual responses to treatments may vary, so consulting with a dermatologist for personalized advice is recommended.